Lymphedema is a pathologic condition that results from a disturbance of the lymphatic system, with localized fluid retention and tissue swelling. Swelling can affect a single limb, multiple limbs, genitalia or the face, abdomen.
Primary lymphedema is a congenital disorder, due to a malformation of lymph vessels and/or nodes (hypotrophic or hypertrophic).
Congenital lymphedema can appear at birth or during the first years of the life. In most of the cases it develops during puberty, perhaps due to the hypotrophy of the lymphatic system which is too small for the growing body, or dysplasia.
Lymphatic anomalies include a variety of developmental and/or functional defects affecting the lymphatic vessels: sporadic and familial forms of primary lymphedema, chylothorax and chylous ascites, lymphatic malformations, and overgrowth syndromes with a lymphatic component.
Germline mutations have been identified in at least 20 genes that encode proteins acting around VEGFR-3 signaling but also downstream of other tyrosine kinase receptors. These mutations exert their effects via the RAS/MAPK and the PI3K/AKT pathways and explain more than a quarter of the incidence of primary lymphedema, mostly of inherited forms. More common forms may also result from multigenic effects or post-zygotic mutations.
DIAGNOSIS
The clinical aspect and the history are important.
Complementary Investigations
Nowadays, radiological evaluation of lymphedema patients can be done through lympho MRI.
PDE (Photodynamic eye) provides information on the superficial lymphatic network.
Magnetic Resonance Lymphography (MRL), with T3 weighted imaging, allows visualization of the lymphatic system anatomy with greater sensitivity than lymphoscintigraphy, without the need of any injection.
Physiotherapic Treatment
Physiotherapy (manual drainages, pressotherapy, compression, bandages) is the usual treatment for chronic lymphedema. It is not a curative therapy, but helps to control the evolution of the disease.
Surgical Treatment
ALNT Indication
Patients with HYPOPLASIA of the lymphatic system, pain and chronic infections are the preferred candidates for the procedure.
The flap is inserted in the area where the nodes and the lymphatic vessels are insufficient.
The healthy nodes contain a growth hormone (VGEF 3) witch induces neoformation of lymphatic ducts. They also help fighting again infections.
In patients with distal lymphedema :
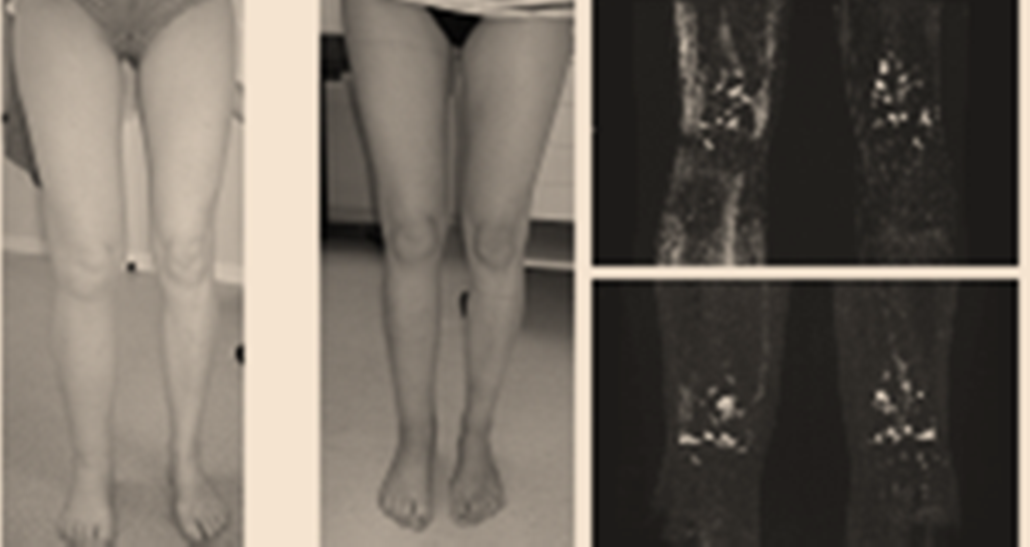
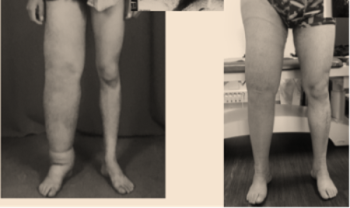
- all patients showed a reduction of the circumference of the treated limb with normalization in 46%
- 88% of the patients had no more infections in the follow-up period.
In patients with generalized limb lymphedema although improvements in limb perimetry were present in 98% of the patients, only 20% of them achieved complete normalization
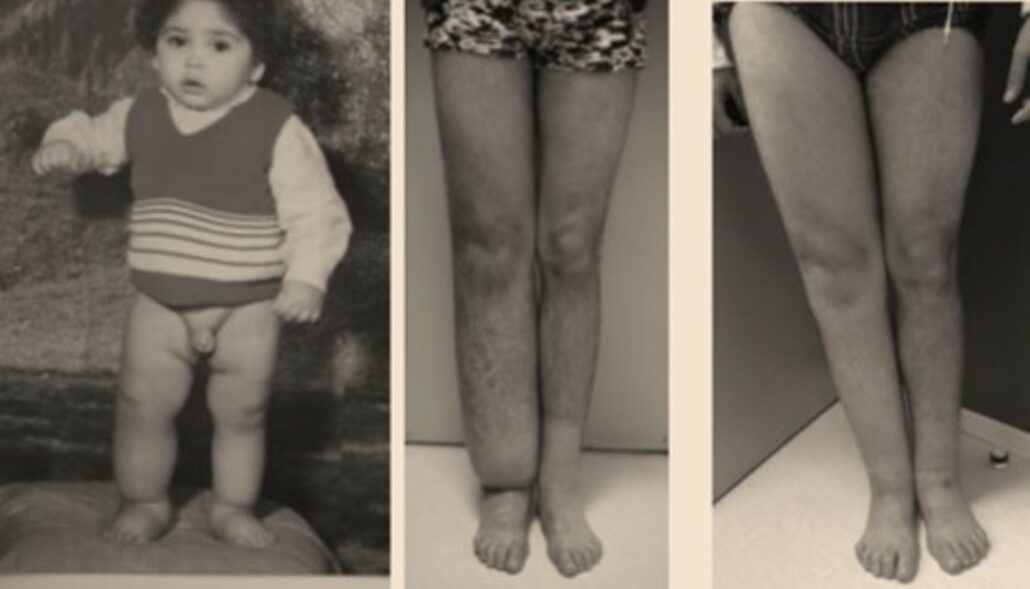
Results 2 years after 2 lymh nodes transplant on a boy who suffered from congenital lymphedema for 19 years.

LYMPHOVENOUS ANASTOMOSIS
In the hyperplasic cases, the high pressure on the lymphatic system can be deviated by lymphovenous bypass. This is the case for patients diagnosed with blockage or absence of the thoracic duct.
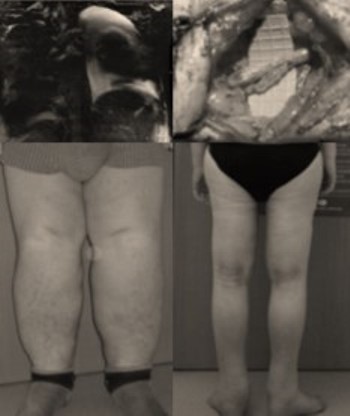
EXCISIONS
Excisions are sometimes necessary to remove the folds, where mycosis are sources of many infections and make the bandages very difficult.
The addition of lymph nodes transfer is very useful to prevent recidive.
EXTENSIVE CONGENITAL LYMPHOEDEMA
Primary lymphoedema can concern Hemi body lateral , inferior, superior, the lungs.It also can present different fibrotic forms.
In those cases, the treatments will combine diet (short chains of lipids), lymphovenous anastomosis in chylothorax pathologies, excisions, combined in some cases with lymphnodes transplantations in hypoplasic cases
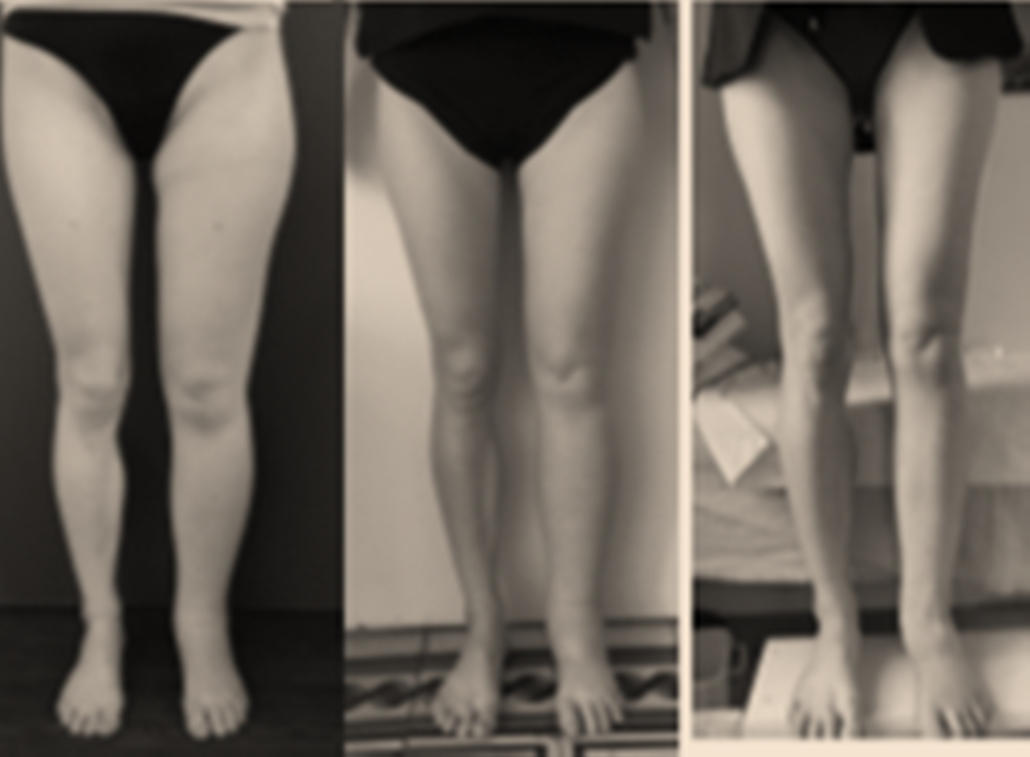
CONGENITAL LYMPHOEDEMA IN UPPER EXTREMITIES
In hypoplasic cases, lymphnodes transfer are proposed with excellent results. Combination with some mocalized liposculptures can be finish the results